Want to know more?
After reading the information on this website, you may wish to explore ECT in more depth. It’s always a good idea to consult multiple, reliable sources. This section offers a selection of further resources. Do you prefer to read more? Or would you rather watch and listen to information? Or perhaps you want to dive into the scientific data on ECT? Follow the links in this section.
Read more about ECT
- Medisch Contact – ECT verdient beter imago – 2009 (Dutch)
- Medisch Contact – Nederlands onderzoek laat zien`: ECT is veilig – 2024 (Dutch)
- Hersenstichting (Brain Foundation – Dutch)
- Depressie vereniging (Depression Association – Dutch)
- Stichting MIND (Dutch)
Watch and listen more about ECT
Scientific references about ECT
- Dutch guideline for ECT
- Website of the Dutch ECT consortium
- Loef et al. (2024) A prediction model for electroconvulsive therapy effectiveness in patients with major depressive disorder from the Dutch ECT Consortium (DEC)
- Loef et al. (2024). Pre-treatment predictors of cognitive side-effects after treatment with electroconvulsive therapy in patients with depression: A multicenter study. PMID: 38195009.
- Dols A, Stek ML. (2009) Elektroconvulsietherapie: indicaties, effectiviteit, veiligheid en bijwerkingen. Ned Tijdschr Geneeskd. 2009;153:A588. Dutch. PMID: 19900318.
- Rovers et al. (2025). Exploring the Decision-Making Process for Electroconvulsive Therapy in Patients With Major Depressive Disorder and Their Relatives After Treatment. J ECT. PMID: 39998858.
- Obbels J et al. (2017) ECT-Related Anxiety: A Systematic Review. The Journal of ECT 33(4):p 229-236.
Veelgestelde vragen
Frequently Asked Questions
This section contains frequently asked questions about ECT. These questions have been gathered from patients, their families and healthcare professionals.
How effective is ECT?
ECT is a safe and effective treatment for mood disorders and psychotic disorders. Among patients with depression who did not respond well to other treatments, more than half make a full recovery after ECT. Others experience a reduction in symptoms but do not become completely symptom-free. A small number of patients notice no improvement. You can read more about this in the section on electroconvulsie therapy.
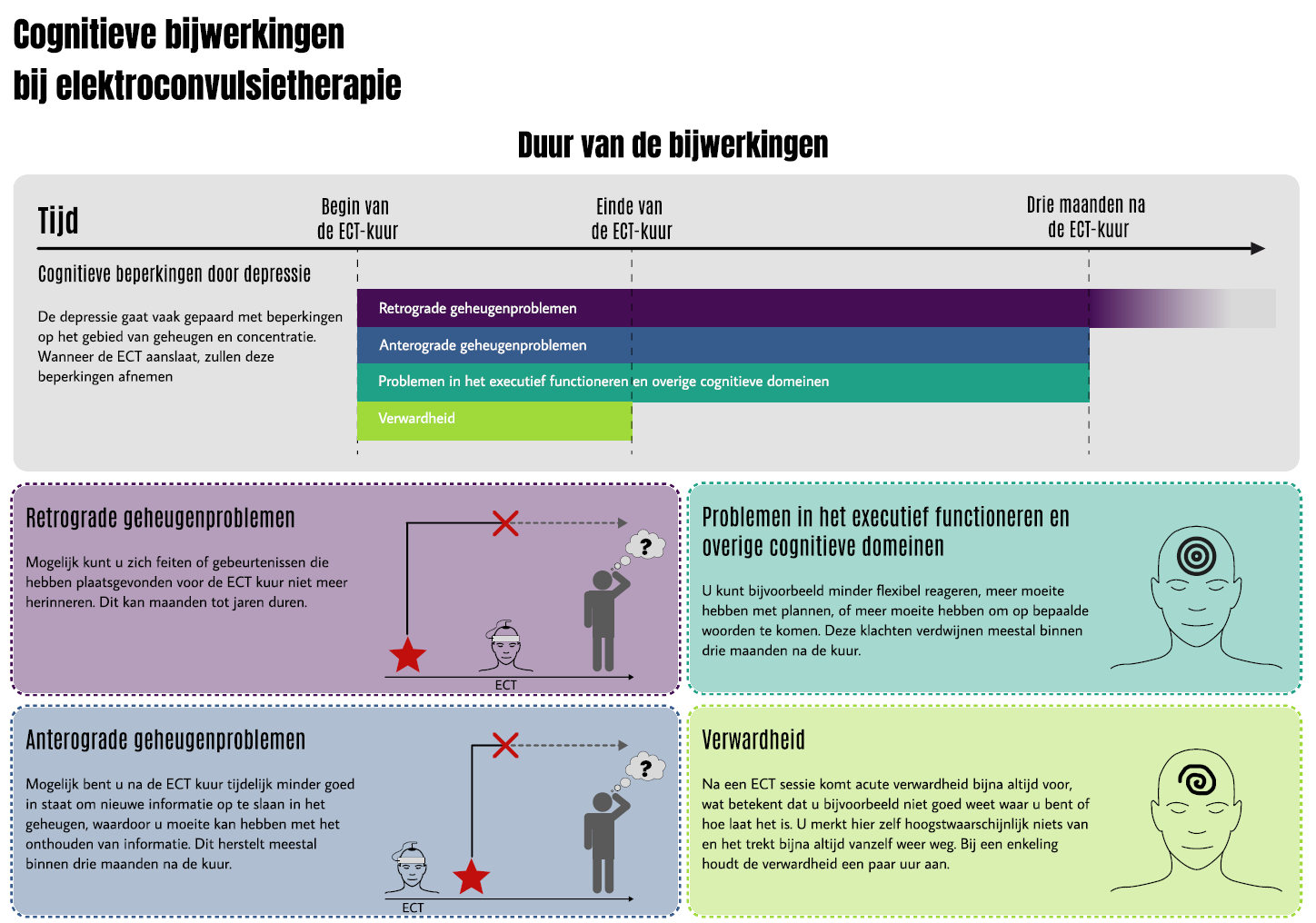
What are the side effects of ECT?
ECT can have both short-term and long-term side effects. Short-term effects typically occur during or immediately after treatment and may include headaches, muscle aches and temporary confusion. Long-term effects may involve memory problems, although not everyone experiences them. You can read more about this on the side effects page.
Which conditions can ECT treat?
ECT is an effective treatment for severe depression, bipolar disorder and psychotic disorders such as schizophrenia. It can also be a valuable option for people with treatment-resistant depression, meaning previous medication and/or psychotherapy has not been effective enough. In addition, ECT can be used in urgent, life-threatening situations such as (malignant) catatonia, acute suicidal crisis or status epilepticus.
What happens during an ECT session?
At the start of treatment, ECT is usually given twice a week. On treatment days, you will go to the ECT centre, where the team will prepare you for the procedure. This usually involves changing clothes, removing jewellery (preferably leaving it at home) and sometimes completing questionnaires. The ECT team will then guide you through the procedure in a structured way. An IV line is placed for administering anaesthesia and a muscle relaxant. Blood pressure cuffs, ECG stickers, EEG electrodes and other sensors are placed on your arms, chest and head. Before starting, the team performs a final “time-out” check to ensure everything is correct. The anesthesiologist then administers the anaesthesia. Once you are under anaesthesia, the treatment is carried out—you will not be aware of anything. The procedure itself only takes a few minutes. If all goes well, you can return home or to your ward about an hour later. Read more about this under electroconvulsive therapy.
Is ECT safe?
Yes, ECT is a safe treatment. Extensive research confirms this. The risk of complications is small. Before starting, patients are carefully screened for any conditions that might make ECT unsafe —such as a large aneurysm, a recent heart attack or a recent stroke. Your psychiatrist, nurses and anesthesiologist work closely together to make both the anaesthesia and the treatment as safe as possible.
Is ECT dangerous or scary?
ECT is not dangerous, so there’s no reason to be afraid—but it can feel intimidating. What feels frightening varies from person to person. For one person, a dark room may feel scary; for another, it might not. Fear of ECT is very common. This fear can be challenging, but it can be addressed. Some people find it helpful to be well-informed beforehand, for example by reading this website. Others prefer to know as little as possible. It’s important to share your feelings with your treatment team and, if possible, talk to someone who has undergone ECT. Doing something relaxing beforehand, such as listening to music, watching a favourite show or practising breathing exercises
How many ECT treatments are needed?
The number of ECT sessions varies depending on the condition and the individual. For depression, an acute course usually involves around 16 treatments. Sessions continue until there has been no further improvement for two weeks. If there is no response, treatment is stopped. In some cases, maintenance ECT is recommended to prevent relapse. This may involve more than 100 sessions spread out over several years.
Is ECT performed under anaesthesia?
Yes. ECT is always done under general anesthesia. The anesthesiologist administers the medication and closely monitors you throughout the procedure. You will not feel or remember anything.
What can I expect after ECT?
After an ECT course, you will need time to recover —this applies regardless of whether the treatment was effective. If symptoms improve, it’s important to start or continue medication to reduce the risk of relapse. The chance of relapse is highest within the first 6–12 months. Psychotherapy or other treatments can also help prevent a return of symptoms. In some cases, ECT is continued at longer intervals as maintenance therapy to help prevent relapse. Discuss with your healthcare provider and loved ones what plan works best for you.
Be aware that ECT can cause side effects. Some people experience memory problems, which can be disruptive in daily life.
These issues usually disappear within 3 months after stopping ECT. Read more about this on the page about side effects.
Can ECT cause permanent memory loss?
Some people experience memory problems after ECT. For most, these fade over time. However, a small percentage of patients experience longer-lasting memory issues —known as permanent memory loss. Permanent memory loss usually affects memories from the time around treatment and sometimes older memories as well. It’s not possible to predict who will experience memory problems or who will have them for a longer period. See the image below for more information about memory issues. More information can also be found on the side effects page.
What does it feel like to undergo ECT?
You won’t feel the treatment itself, since it’s performed under general anaesthesia. If you’d like to know more about how patients experience ECT during and after the procedure, you can read their stories on the experiences page.
Is ECT a last resort?
No. ECT is a safe and effective treatment for various mental and physical health conditions. In some cases, such as severe (psychotic) depression or life-threatening situations, ECT may even be used as the first treatment option. However, in most cases, other treatments such as medication or therapy are tried first, as these are often effective and less intensive. If ECT doesn’t help, there are still other treatment possibilities available. Always discuss the options with your healthcare provider.
How does ECT differ from other treatments for depression?
Depression can be treated in different ways, including psychotherapy, medication and neurostimulation. These approaches can be used separately or in combination. Together with your clinician, you’ll decide which treatment is most suitable. Medication (such as antidepressants) and psychotherapy are both effective and when used together, they often have an even greater impact.
ECT is a type of neurostimulation. It works by stimulating areas of the brain that don’t function properly during depression.
Other forms of neurostimulation include rTMS (repetitive transcranial magnetic stimulation) and DBS (deep brain stimulation).
If you’d like to learn more, visit the page on ECT and the brain.
Can I keep taking my medication during ECT?
In most cases, you can continue taking your regular medication during ECT. However, some medicines may affect how well the treatment works.
- Medications for anxiety (benzodiazepines) en medications for epilepsy (antiepileptics) can reduce the effectiveness of ECT. They increase the stimulation threshold in the brain, making the electrical impulse less effective. In some cases, these medications need to be paused temporarily the day before ECT.
- Lithium may cause increased confusion after ECT. Your clinician may advise temporarily stopping this medication or lowering the dose..
Your clinician will always discuss this with you beforehand. Never stop taking your medication on your own without medical advice. If you have questions, be sure to write them down and discuss them with your clinician.
Glossary
Depressive disorder
A depressive disorder is a condition marked by a prolonged low mood and loss of interest or pleasure in daily activities. Common symptoms include fatigue, sleep problems, appetite changes, difficulty concentrating and feelings of worthlessness or guilt. In some cases, depression may also involve thoughts of death or suicide.
Mania
Mania is a period of abnormally elevated mood, extreme energy and excessive activity. It is a symptom of bipolar disorder and may include inflated self-esteem, reduced need for sleep, fast or incoherent speech, impulsive behaviour and trouble concentrating. In severe cases, mania can lead to psychotic symptoms such as delusions or hallucinations.
Bipolar disorder
Bipolar disorder is a condition characterised by extreme mood swings. These range from manic or hypomanic episodes (high energy, euphoria or irritability) to depressive episodes (low mood, loss of interest and fatigue).
Psychosis
Psychosis is a state in which a person partly or completely loses touch with reality. This can involve delusions (false fixed beliefs) and hallucinations (seeing, hearing, smelling or feeling things that aren’t there). People experiencing psychosis may also think in a confused way, struggle with logical reasoning and react differently to their surroundings. Psychosis can occur in mental health conditions such as schizophrenia, bipolar disorder or depression with psychotic features.
Schizophrenia
Schizophrenia is a disorder in which a person’s connection with reality is disrupted. People with schizophrenia may experience psychoses, with symptoms such as delusions, hallucinations, disorganised thinking and incoherent speech. They may also struggle with emotions, motivation and social functioning.
Psychotherapy
Psychotherapy is a treatment method that uses conversations and therapeutic techniques to relieve symptoms and emotional distress. It helps people better understand and change their thoughts, feelings and behaviour patterns. Psychotherapy can be used for various conditions, including depression, anxiety disorders and personality disorders.
Neurostimulation
Neurostimulation is a medical treatment that uses electrical or magnetic impulses to activate certain areas of the brain or nervous system. It can help in conditions such as depression, epilepsy, chronic pain and Parkinson’s disease. Examples of neurostimulation include deep brain stimulation (DBS), electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS) and vagus nerve stimulation (VNS). By influencing brain activity, these treatments can help reduce symptoms.
Bilateral
Bilateral means “on both sides”. In electroconvulsive therapy, bilateral electrode placement refers to positioning electrodes on both sides of the head, often above the temples. This means that both hemispheres of the brain are stimulated during treatment.
Right unilateral (RUL)
Unilateral means “on one side”. In electroconvulsive therapy, RUL refers to placing the electrodes on the right side of the head, usually above the temple area. With RUL ECT, the electrical current is directed to one side of the brain—in this case, the right hemisphere.



